
The ASAM Pain & Addiction: Common Threads XXIII - 2022
- Registration Closed

Thursday, March 31, 2022
8:00 am – 5:30 pm ET
Live and On-Demand Workshop
Overview
Interdisciplinary care for patients with pain and addiction in the virtual age
The ASAM Pain & Addiction: Common Threads Course is one of ASAM’s longest running and most popular courses. This advanced course increases learners’ understanding of complex topics and improves treatment of patients who fall somewhere in the gray area around pain and addiction. Participants will learn new research developments that affect treatment, and how to integrate these techniques into their own practices. This year’s course will utilize a dynamic mix of teaching methods to engage an advanced audience.
Learning Objectives
Upon completion of this educational activity, participants should be able to:
- Describe new challenges in pain and addiction that have arisen from the COVID-19 pandemic.
- Identify strategies to build resilience among healthcare teams and patients.
- Differentiate between various interdisciplinary care models for treating patients with pain and addiction and explain the purpose of utilizing an interdisciplinary care team.
- Describe common ways patients may be using Kratom as an alternative method for treatment of pain.
- Compare different treatment options for patients who cannot tolerate buprenorphine.
- Implement practical strategies and principles of a successful virtual pain and addiction assessment
- Question the disparities in access to telemedicine that exists within the US and recognize the current and future telemedicine policies that affect patients’ access to treatment.
- Recognize the complex relationship between stimulants and chronic pain.
- Assess the current fentanyl epidemic and discuss promising treatment and harm-reduction practices.
- Compare key pain and addiction research publications from 2021-2022 and identify their relevance to practice.
Fees
| Rate Description | Rate |
| ASAM Member | $149 |
| Non-Member | $199 |
| Associate Member | $99 |
| Resident Member* | $99 |
| Student Member* | $99 |
(*) Residents, Fellows-in-training, Interns, and Students must join ASAM to receive a discounted registration rate.
- Click here to become an ASAM member.
- Residents, Fellows-in-training, and Interns: National and Chapter membership dues apply.
- There is no charge for Students to become a Member, but verification of student status is required.
- Membership Question? Call ASAM at 1.301.656.3920, email us, or view the ASAM website for more information.
Refunds & Cancellations
All ASAM e-Learning Center refund requests must be made in writing to education@asam.org within 90 days of purchase. Those requesting refunds for courses that are in progress will receive partial refunds or e-Learning Center credit. Automatic full refunds will be made for any course with a live-course component that has been cancelled.
Registration Deadline: 04/30/2024
Get Started
To begin, click on the Contents tab to get started with the course. Click on the other tabs to view information on the presenters, credit and disclosures, how to claim credits and certificate, and materials/resources related to the course.
Claim Credit & Certificate
- If you attended the live course, skip to step 4. If viewing the On-Demand course, go to step 2.
- Click the Contents tab, expand the section of the video you would like to view, then select View On-Demand Recording. After viewing the entire video, return to the Contents tab.
- Click Complete Post Test to answer quiz questions. After completing the quiz, return to the Contents tab.
- Click Complete Evaluation to answer evaluation questions. Scroll down on all questions, there are answers that expand past the size of the window. Submit the evaluation (the next box should activate, and the evaluation box should turn green with a white check mark).
- Click the button “Claim Credits” in the box titled “Claim Credits & Certificate." Choose the type of credit and click submit. Click the button “View/Print Certificate” to save or print your certificate. If you ever lose your certificate, you can come back to the ASAM e-Learning Center and view it on your transcript (found in the Dashboard).
Need Assistance?
If you have are experiencing any log in issues, cannot access a course, need assistance claiming credit, or have other questions or concerns, please e-mail Education@asam.org for assistance.
For learners who may have difficulty typing, moving a mouse or reading, Essential Accessibility is an application available for use to assist.

Barbara Marie, PhD, AGPCNP, FAANP, FAAN
Assistant Professor College of Nursing
University of Iowa
Barbara St. Marie is a certified Adult, Gerontology, Primary Care Nurse Practitioner, Pain Management Certified through ANCC, and Assistant Professor at the University of Iowa College of Nursing. She is a Fellow in the American Association of Nurse Practitioners, and a Fellow in the American Academy of Nursing. Dr. St. Marie has a PhD from the University of Wisconsin, Milwaukee, and completed Postdoctoral studies in Pain and Associated Symptoms at the College of Nursing, University of Iowa from 2012-2014. She has been editor of the first and second edition of the Core Curriculum for Pain Management Nursing through the American Society for Pain Management Nursing. As Principal Investigator on three grants, her research focuses on patients with pain receiving opioids, experiences and decision making for all prescribing healthcare providers, and in looking at alternative means of managing pain and risk for opioid use disorder. Dr. St. Marie is now the PI on a study funded through the National Institute of Health -- National Institute on Drug Abuse entitled, Decision Support for Responsible Pain Management.
No relevant financial disclosures.

Matthew Herbert, PhD
Research Psychologist and Assistant Professor of Psychiatry
VA San Diego Healthcare System and University of California San Diego, California
Matthew Herbert, PhD, is a Research Psychologist at the VA San Diego Healthcare System and Assistant Professor in the Department of Psychiatry at University of California San Diego. Dr. Herbert's research program consists of elucidating biopsychosocial factors that underlay the maintenance and severity of chronic pain and the development and evaluation of mindfulness-based treatments for chronic pain. An additional focus of his research is compassion; specifically, novel strategies for measuring compassion and the impact of contemplative compassion practice on treatment outcomes. Dr. Herbert also is a licensed clinical psychologist and a clinical supervisor in the Clinical Psychology Joint Doctoral Program at UCSD and San Diego State University.
No relevant financial disclosures.

Aram Mardian, MD
Aram Mardian, M.D. is a clinical associate professor of Family, Community, and Preventive Medicine at the University of Arizona College of Medicine–Phoenix is a board-certified family physician and holds additional certifications in addiction medicine, pain medicine, and medical acupuncture. He is the founding Chief of the Chronic Pain Wellness Center at the Phoenix VA Health Care System, which models interprofessional whole-person care for patients with pain and opioid use disorder. Dr. Mardian serves as Co-Chair for the Arizona Pain and Addiction Curriculum Workgroup.
No relevant financial disclosures.

Daniel Vilaubi, DPT
Physical Therapist
Chronic Pain Wellness Center, Phoenix VA Health Care System
Dr. Vilaubi is a Physical Therapist at the Phoenix VA within the Chronic Pain Wellness Center. He is a Fellow of the American Academy of Orthopaedic Manual Physical Therapists and was a sergeant in the United States Marine Corps. He specializes in movement therapy and pain neuroscience education for both individual and group treatment. Dr. Vilaubi’s professional interests include narrative medicine, leadership development, and high-performance coaching.
No relevant financial disclosures.

Eric Hanson, PhD
Pain Psychologist; Program Manager
Chronic Pain Wellness Center Phoenix VA Health Care Center
Dr. Hanson is a Pain Psychologist at the Phoenix VA within the Chronic Pain Wellness Center and is the Pain Psychology Program Manager. They are a Assistant Profession at University of Arizona College of Medicine – Phoenix (UA COM-P). They are a VA National Trainer and Consultant for CBT-CP and they give a variety of trainings and consultations throughout the year to bolster pain treatment within the VA. In addition, Dr. Hanson teaches, supervises, and mentors Addiction Medicine Fellows and Psychology Interns/Fellows in evidence based treatment for pain and addiction. They are well versed in a variety of treatments for chronic pain as well as understanding the importance of good clinical assessment of addiction within the context of pain management. Dr. Hanson’s professional interests include sociopsychological aspects of pain and addiction as well as intersectionality of diversity factors influencing pain and addiction treatment.
No relevant financial disclosures.

Bethany DiPaula, Pharm.D., BCPP, FASHP
Professor
University of Maryland, School of Pharmacy
Bethany A. DiPaula, Pharm.D., BCPP, FASHP is professor at the University of Maryland, School of Pharmacy and a consultant with School of Medicine Maryland Addiction Consultation Service (MACS). Dr. DiPaula is a residency trained, board certified psychiatric pharmacist with a passion for managing patients with substance use disorders (SUD). Dr. DiPaula practices with a medical group in Baltimore City providing medication management services for patients diagnosed with SUD and other psychiatric disorders. She is active in shaping state collaborative drug therapy management (CDTM) practice. She created pharmacist medication management practices for indigent patients with SUD and has lectured and published on these experiences. Dr. DiPaula worked with a state legislative committee to allow for expanded access to naloxone through pharmacist dispensing using a state standing order. She has educated over 900 county residents about overdose management and received a grant to provide opioid use disorder academic detailing to community pharmacists. Dr. DiPaula is the University of Maryland PGY2 Psychiatric Pharmacy Residency Program Director and volunteers as an American Society of Health-System Pharmacists (ASHP) accreditation guest surveyor. She recently served on the ASHP Opioid Taskforce. She has served as the Chairperson for the College of Psychiatric and Neurologic Pharmacists (CPNP) Substance Abuse Taskforce and Substance Use Steering Committee. She just completed her second term on the Board of Pharmacy Specialties (BPS) Specialty Council on Psychiatric Pharmacy.
No relevant financial disclosures.

Anita Karnik, MD
Addiction Psychiatrist
Phoenix VA Health Care System
Anita Karnik M.D. is the program director for University of Arizona College of Medicine Phoenix Addiction Medicine Fellowship. She is an addiction psychiatrist at the Phoenix VA Health Care System and practices in an integrated pain and addiction chronic pain and wellness center. She received her M.D. at Texas A&M College of Medicine and completed her general and child and adolescent psychiatry training though the Baylor Scott and White Psychiatry Residency Program. Dr. Karnik went on to further specialize in addiction psychiatry at the University of Cincinnati Addiction Psychiatry Fellowship. Dr. Karnik specializes in caring for patients who have co-occurring chronic pain, substance use disorders, and mental health concerns. She is passionate about destigmatizing addiction care. Dr. Karnik enjoys teaching and encourages medical students, residents, and fellows to partner with their patients and approach addiction care from an integrated whole person approach.
No relevant financial disclosures.

Pamela Pentin, MD, JD, FAAFP
Associate Professor
University of Washington School of Medicine, Washington
Pamela Pentin, M.D., JD, FAAFP is an Associate Professor in the Department of Family Medicine at the University of Washington School of Medicine in Seattle, where she teaches residents and medical students. She is chief of service for family medicine at the UW Medical Center. She is a graduate of Sidney Kimmel Medical College of Thomas Jefferson University, and completed her residency in family medicine at the University of Vermont, where she also served as chief resident.
Dr. Pentin is a full scope family physician, including obstetrics and hospital medicine, but her area of focus within primary care is substance use disorders. A waivered Buprenorphine prescriber since 2004, she has extensive experience managing acute and chronic pain, opioid use disorder, and the intersection between them. Her office-based practice rapidly shifted to a mostly Telehealth format at the start of the COVID pandemic, and she learned much from trial and error with thay move to virtual medicine. Dr. Pentin is also the primary care leader of UW Telepain, a weekly video-conference-based knowledge network providing guidance managing challenging pain and addiction patients to providers throughout the Pacific Northwest and beyond.
No relevant financial disclosures.

Vania Rudolf
MD, MPH, DFASAM
Vania Rudolf, MD, MPH, DFASAM is a family and addiction medicine physician who is providing care to pregnant and parenting women with substance use disorder. She has a background in family medicine with OB and has completed Fellowships in Integrative Medicine, Addiction Medicine and High Risk Obstetrics at Swedish Medical Center. She has earned public health training at the UW. Dr. Rudolf continues to be a compassionate advocate for improving kind non-judgmental services and removing barriers to care. Providing compassionate trauma-responsive care to vulnerable women, babies and families is the primary focus of her practice in addition to clinical research related to clinical outcomes for substance use disorder, transition to MAT and prescribing policies to optimize safe and adequate postpartum analgesia management. She is the Medical Director for Addiction Recovery Services at Swedish Medical Center, an assistant professor at University of Washington, Seattle, WA and the Chair for the National Womens' Addiction Group related to the American Society of Addiction Medicine. She serves on the maternal mortality review board for the state of Washington and has many years as a practicing clinician.
No Relevant Financial Disclosures

Mollie B. Nisen, MD
Fellow
Addiction Recovery Services, Swedish Medical Center
Mollie Bea Nisen, MD (she/her) is a current fellow with the Swedish Addiction Medicine program in Seattle, Washington. After graduating from Albert Einstein College of Medicine in the Bronx, NY, Mollie completed her residency training as one of the Chief Residents of the Swedish Cherry Hill Family Medicine program. She maintains a full spectrum primary care practice with particular interest in primary and obstetrical care for patients with substance use disorder and the intersection of reproductive justice and harm reduction in addiction medicine. Mollie has a background in community organizing and strives to ground her clinical work in social justice and antiracist praxis.
No relevant financial disclosures.
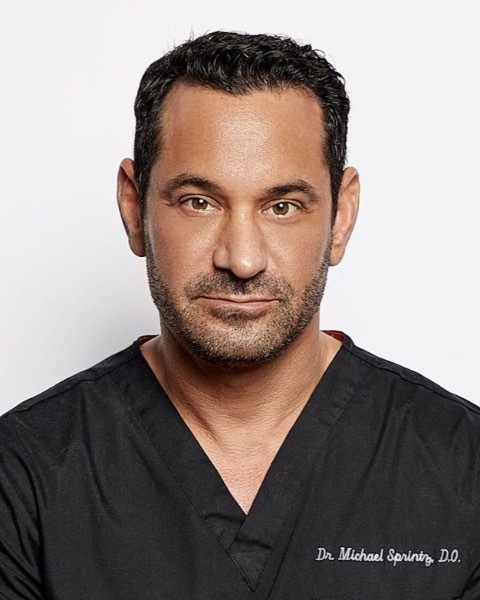
Michael Sprintz DO, DFASAM
Founder and CEO
Cellarian/Sprintz Center for Pain
Michael Sprintz, D.O. received his medical degree from Midwestern University-Chicago College of Osteopathic Medicine in 1997 and went on to a residency in Anesthesiology at Johns Hopkins Hospital. He left Hopkins to do post-doctoral research in biomedical nanotechnology before returning to complete his anesthesia training at University of South Florida. Dr. Sprintz completed a Pain Medicine Fellowship at MD Anderson Cancer Center in 2012 and is triple-board-certified in Anesthesiology, Addiction Medicine, and Pain Medicine. Dr. Sprintz is the Past-President of the Texas Society of Addiction Medicine, as well as the CEO of iLumHealth, a software company developing world-class products to prevent abuse and diversion of prescription drugs, educate providers, and employ rational solutions that save lives and create value. In addition, Dr. Sprintz is the Founder and Chief Medical Officer of the Sprintz Center for Pain and Dependency, an ultra-specialized outpatient center for the comprehensive treatment of chronic pain, dependency and addiction, located in The Woodlands, TX.
Does Disclose - MPS consulting and media, LLC: pain, addiction and technology consulting, managing partner, Revelliance, llc: healthcare revenue cycle technology development, FDA analgesic and anesthetic drug products, advisory committee, Sprintz center for pain, pllc. (medical practice), employment, Sprintz center for recovery, pllc. (medical practice), employment, Cellarian, inc. (healthcare related software company), employment, Cellarian holdings, inc. (owns cellarian, inc.), board member, Spark biomedical: (medical device company), consultant, Assurance med management, llc (healthcare software company), consultant, Saluda medical (medical device company), consultant, Nanomedical systems, inc. (biomedical nanotechnology company), consultant.

Stephanie T. Weiss
MD, PhD
Stephanie T. Weiss, MD PhD is the staff Research Physician serving the Translational Addiction Medicine Branch (TAMB) of the NIDA Intramural Research Program. After earning a Ph.D. in pharmaceutical chemistry, Dr. Weiss received her medical degree from Cleveland Clinic Lerner College of Medicine. She is board certified in emergency medicine and medical toxicology, a subspecialty that cares for patients with poisonings, environmental exposures, and overdoses. She subsequently completed a second fellowship in addiction medicine research and was selected to participate in the Boston University Research in Addiction Medicine Scholars Program prior to joining NIDA. Dr. Weiss assumes responsibility for providing optimal, safe, and ethical care to study participants and clinical support toward the TAMB mission conducting inpatient and outpatient proof-of-concept human laboratory studies. Her research interests include novel psychoactive substances, medication misuse, and improving interpretation of urine drug testing.
No relevant financial disclosures.

Phillip O. Coffin, MD, MIA, FACP, FIDSA
Director of Substance Use Research
San Francisco Dept of Public Health
Phillip Coffin, MD, MIA, is a board-certified, practicing internist, infectious disease, and addiction medicine specialist, including inpatient and outpatient care. Dr. Coffin also directs the Center on Substance Use and Health, where he conducts and oversees clinical trials addressing therapies for substance use disorders and prevention or treatment of overdose, HIV, and viral hepatitis; observational studies addressing substance use and the shifting climate of opioid prescribing; local substance use epidemiology; and programmatic efforts to improve opioid management in clinical care.
Does Disclose Gilead Sciences: NIH-funded trial of PrEP that receives donated TAF/(PrEP), Clinical Condition: HIV.

Marianne Fingerhood, DNP, ANP-BC
Marianne Fingerhood has been a nurse for over 35 years. Her career began at the bedside in Cardiac Critical Care and continued as a staff educator. She has been a nurse practitioner in adult primary care for more than 20 years and a clinical preceptor and nursing instructor for the past 19 years. In all settings, she has brought a passion for education, whether it be with patients, students, or colleagues. As a nurse practitioner with Johns Hopkins Community Physicians, she collaborates with other members of the health care team to promote excellence in prevention and management of chronic illness and patient education. Her areas of interest are safe opioid prescribing, identification and treatment of opioid use disorder, and the support and education of nurse practitioners as they transition into their roles as primary care providers. In July 2020, she received a grant from the Maryland Higher Education Commission to begin a Primary Care Nurse Practitioner Fellowship.
No relevant financial disclosures

Laura M. Frankart, PharmD, MEd, BCPS
Associate Professor
Virginia Commonwealth University
Laura Morgan Frankart is currently Director of Education and Assessment and Associate Professor in the Department of Pharmacotherapy and Outcomes Science at Virginia Commonwealth University/Medical College of Virginia. She works as a clinical pharmacist in palliative care at VCU Health Massey Cancer Center. She previously worked for 9 years in the Primary Care Pain Clinic in the MCV Physicians Internal Medicine clinic. She has co-authored publications related to using opioid risk screening tools and prescription monitoring programs in practice and unintentional prescription opioid overdose.
No relevant financial disclosures.

Emanuel N. Husu, MD
Assistant Professor, Physical Medicine & Rehabilitation
Baylor College of Medicine
Emanuel N. Husu, M.D. is currently an Assistant Professor of Physical Medicine & Rehabilitation at Baylor College of Medicine where he integrates addiction medicine into his interventional pain management practice, the latter of which consists mainly of spine medicine, but also includes headache, abdominal pain, musculoskeletal pain management. He received his bachelor’s degree from the University of California, Irvine. He spent some time after that conducting brain cancer research and ketogenic diet research related to pediatric epilepsy. He then went on to obtain his medical degree from the University of Arizona School of Medicine Tucson. He completed his internship at Abington Hospital - Jefferson Health and residency in physical medicine and rehabilitation at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Husu then completed a pain medicine fellowship in the Departments of Rehabilitation Medicine and Anesthesiology at the University of Minnesota. Following his pain medicine fellowship, he worked for two years as an interventional pain physician in the Chicagoland area during which he was confronted with a disturbingly high prevalence of substance abuse among his patients, in particular that of prescription opioids. This prompted him to complete an addiction medicine fellowship at Loyola University Chicago Stritch School of Medicine.
No relevant financial disclosures.

Gregory Rudolf
MD, DFASAM
Dr Rudolf is a physician board certified in addiction medicine, pain medicine, medical acupuncture and family medicine practicing at Swedish Pain Services in Seattle. The clinic integrates multidisciplinary pain care approaches in an effort to optimize patient functional outcomes and self-efficacy. He has also worked extensively in inpatient substance use disorder treatment settings and has published on the topic of opioid withdrawal management. He is the current Chair of the ASAM Pain and Addiction Committee, the immediate past president of the Washington Society of Addiction Medicine, and is a clinical associate professor at University of Washington.
No relevant financial disclosures.
CME, CE, CEU and Other Credit Types

ACCME Accreditation Statement
The American Society of Addiction Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA Credit Designation Statement
The American Society of Addiction Medicine designates this live activity for a maximum of 8 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
American Academy of Family Physicians (AAFP)
The AAFP has reviewed The ASAM Pain & Addiction: Common Threads Course XXIII and deemed it acceptable for up to 8.00 Live AAFP Prescribed credits. Term of Approval is from 03/31/2022 to 03/31/2022. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
American Academy of Physician Assistants (AAPA)
This activity has been reviewed by the AAPA Review Panel and is compliant with AAPA CME Criteria. This activity is designated for 8 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation. Approval is valid from 3/31/2022 to 3/31/2023. AAPA reference number: CME-204636.
American Association of Nurse Practitioners (AANP)
This activity is approved for 8.0 contact hour(s) of continuing education (which includes 2.75 hour(s) of pharmacology) by the American Association of Nurse Practitioners®. Activity ID# 22025347. This activity was planned in accordance with AANP Accreditation Standards and Policies.
NAADAC, the Association for Addiction Professionals
This activity has been approved by the American Society of Addiction Medicine, as a NAADAC Approved Education Provider, for educational credits. NAADAC Provider #295, ASAM is responsible for all aspects of the programming.
California Association for Drug/Alcohol Educators (CAADE)
This educational program is approved by CAADE: #CP40 999 1225
California Association of DUI Treatment Centers (CADTP)
This educational program is approved by CADTP: #205
California Consortium of Addiction Programs and Professionals (CCAPP)
This educational program is approved by CCAPP: #OS-20-330-1224
Continuing Education Credits (CEUs)
Non-physician participants will receive a certificate of attendance upon completion of the activity and an online evaluation confirming their participation. Participants should submit his/her certificate of attendance to their professional organization/institute.
Maintenance of Certification
American Board of Medical Specialties (ABMS)
Through the American Board of Medical Specialties (“ABMS”) ongoing commitment to increase access to practice relevant Continuing Certification Activities through the ABMS Continuing Certification Directory ASAM Pain & Addiction: Common Threads Course XXIII has met the requirements as a MOC Part II CME Activity (apply toward general CME requirement) for the following ABMS Member Boards: Allergy and Immunology, Anesthesiology, Family Medicine, Physical Medicine and Rehabilitation, Psychiatry and Neurology, Preventive Medicine, Radiology
American Board of Preventive Medicine (ABPM)
The American Board of Preventive Medicine (ABPM) has approved this activity for a maximum of 8 LLSA credits towards ABPM MOC Part II requirements.
American Board of Anesthesiology (ABA)
This activity contributes to the CME component of the American Board of Anesthesiology’s redesigned Maintenance of Certification in Anesthesiology TM (MOCA®) program, known as MOCA 2.0®.
American Board of Pediatrics (ABP)
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn a maximum of 8 MOC points in the American Board of Pediatrics’ (ABP) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABP MOC credit.
American Board of Internal Medicine (ABIM)
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 8 Medical Knowledge MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credits.
American Board of Surgery (ABS)
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME and/or Self-Assessment requirements of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
American Board of Psychiatry and Neurology (ABPN)
Successful completion of this CME activity can be used to satisfy the American Board of Psychiatry and Neurology’s (ABPN) CME requirement for Maintenance of Certification program
American Board of Addiction Medicine (ABAM)
Successful completion of this activity can be used to satisfy the American Board of Addiction Medicine (ABAM) for Tmoc as credits towards ABAM LLSA Part II requirements.
Royal College of Physicians and Surgeons of Canada (RCPSC)
Royal College Fellows can use participation in Accredited Continuing Medical Education to earn Section 3 Credits.
Acknowledgement
This content has been made available in part by a small unrestricted educational grant from Heron Therapeutics. No input or influence from Heron Therapeutics was included in the development of the educational content. As an ACCME Provider, ASAM follows the ACCME Standards for Integrity and Independence for Accredited Continuing Education stating that owners and employees of ineligible companies are excluded from participating as planners or faculty, and must not be allowed to influence or control any aspect of the planning, delivery, or evaluation of accredited continuing education
Disclosure Information
In accordance with disclosure policies of ASAM and the ACCME, the effort is made to ensure balance, independence, objectivity, and scientific rigor in all CME/CE activities. These policies include mitigating all possible relevant financial relationships with ineligible companies for the Planning Committees and Presenters. All activity Planning Committee members and Faculty have disclosed relevant financial relationship information. The ASAM CE Committee has reviewed these disclosures and determined that the relationships are not inappropriate in the context of their respective presentations and are not inconsistent with the educational goals and integrity of the activity.

